When Speed Saves Lives
More often than not, it takes years before patients can benefit from a breakthrough in medical research. Now, the Robert Bosch Stiftung is looking to change this – more specifically, by promoting translation: the rapid transfer of research findings into successful treatments. Just how this principle works in practice is clear on a daily basis at the Bosch Health Campus.
Cancer is never good news, and Melanie Sonnleitner (name changed by the editing team) was no exception. Plagued by an increasingly persistent cough, the then 58-year-old from Stuttgart was diagnosed with bronchial carcinoma, and things quickly went downhill. “The never-ending dry cough, soon joined by pain, was like torture, but above all there was this terrible sense of fear.” A marathon of hospital visits followed: immunotherapy, cytostatic therapy (more commonly known as chemotherapy), and later maintenance therapy. But nothing quite cracked it.
A year after her diagnosis, Sonnleitner could barely leave her bed, suffering from severe shortness of breath and having developed abdominal metastases. “Really, we had pretty much exhausted all avenues of treatment,” recalls Prof. Dr. Hans-Georg Kopp, Head Physician of Pneumological Oncology and Molecular Oncology at the Robert Bosch Hospital in Stuttgart. German medical jargon even has a term for this: “austherapiert”, or “therapied out”. But the hospital team had one last trick up their sleeve.
In the summer of 2021, tumor tissue was removed from Ms. Sonnleitner over the course of three attempts. Only the last, a bronchoscopy, proved successful, but it was all worth it. The tumor’s RNA was examined in the laboratory. “In the process, we discovered what’s known as an RET fusion: a genetic mutation present in less than one percent of lung cancer cases,” explains Prof. Kopp.
Right about the same time, a new drug for precisely that tumor variant was emerging on the market, which targeted the mutation within the tumor. Two years after her initial diagnosis, Ms. Sonnleitner once again started on a new drug: selpercatinib, an inhibitor that turns the tumor’s strength, namely its ability to alter the RET gene, into its Achilles heel. And this time, it was all about to change.
The process behind Ms. Sonnleitner’s case is called “translation”. This refers to the rapid transfer of medical research into real-life clinical treatments. The gene fusion seen in the type of bronchial cancer Ms. Sonnleitner suffers from was discovered only a few years ago – and yet a targeted treatment is already available. Of course, you would be forgiven for thinking that the latest findings from research would normally reach patients as quickly as possible. But unfortunately this is rarely the case.
The primary reason behind this is that these days, drug development is really only carried out by large corporations. Conversely, the links between these processes and core research, which is vitally important, are often missing. One group is conducting research into the biochemical foundations of life, while another entirely is manufacturing products for a specific market. And all this is happening in individual ‘bubbles’, each separated from the other in terms of both staff and space. The result is that a whole host of potentially life-saving research never even reaches the patients that need it or, when it does, it’s already too late.
"We can investigate how drugs work on the body, how they interact with one another and, above all, how they interact with different genetic make-ups."
Translating research into results
Now the Dr. Margarete Fischer-Bosch Institute for Clinical Pharmacology (IKP) at the Robert Bosch Hospital wants to change this, ensuring that medical innovations help as many people as possible as quickly as possible. And it’s just walking distance from the oncology department.
“We have seen incredible progress in cancer treatments in recent years, especially in the field of pharmacogenomics, or cancer treatments that are specific to an individual’s germline or the tumor’s genome,” explains Prof. Dr. Matthias Schwab, the Institute’s director since 2007 and the chair of Clinical Pharmacology at the University of Tübingen.
“Theoretically speaking, many cancers can now be cured or converted into a chronic disease. It’s truly terrible when sufferers live with a chance of being cured but also the knowledge that time is running out.” The way Prof. Dr. Schwab sees it, doctors and researchers have a moral obligation to ensure that findings are translated into results quickly.
Schwab sits in a cramped office on the third floor of the IKP. On the walls are the posters he has presented at recent specialist conferences, showing color-coded tumors at various stages. Here at the IKP, research is conducted over five floors, with around 80 people working here, many in doctoral or postdoctoral positions.
“We don’t usually develop new drugs,” says Prof. Schwab, detailing the Institute’s approach, “but we can, for example, investigate how drugs work on the body, how they interact with one another and, above all, how they interact with different genetic make-ups – whether that’s from an individual or a tumor.”
The IKP
In 1973, the Dr. Margarete Fischer-Bosch Institute for Clinical Pharmacology was founded, named after Bosch's eldest daughter, who made this possible with a donation. At the beginning, four employees researched how the type and timing of medication administration affected the success of therapy - and how patients could best benefit from it. Today, with around 80 employees, the IKP is the largest scientific research unit in the field of clinical pharmacology in Germany.
One example of the IKP’s pioneering work is in the treatment of breast cancer, the single most common cancer to affect women. For a long time, breast cancer was also treated using cytostatics. But this treatment, which, broadly speaking, inhibits the growth of all cells in the body, is enormously taxing, with hair loss, nausea, and severe pain all common side effects.
As early as the 1960s, researchers had already discovered a different mechanism for combating breast cancer: the substance tamoxifen, which interferes with the patient’s estrogen balance and can lead to the tumor disappearing entirely. It was a truly groundbreaking drug – but sadly not for all patients. “My predecessor here at the IKP, Prof. Dr. Michel Eichelbaum, discovered the CYP2D6 polymorphism back in 1975,” explains Schwab.
This variation means that between ten and twenty percent of women are genetically missing the enzyme which first metabolizes tamoxifen into an effective substance in the body. As such, the drug is of little use to them, and the tumor can still grow. What can help these women, however, is instead administering the metabolite to them directly – an option that has been on the market for several years now.
How a tumor avatar saves lives
Researchers at the IKP are fighting cancer on a whole range of levels. “You need to work with models to really understand the metabolism of tumors, for example how they respond to drugs,” says Dr. Thomas Mürdter, the Institute’s deputy director. For a long time, tumor tissue was cultivated in Petri dishes for this reason. The problem is that tumors are incredibly complex structures where the tumor cells are interacting with the surrounding tissue, including blood vessels, fibroblasts and immune cells. A 2-D model in a dish just isn’t capable of replicating this level of complexity. Instead, the team, led by Dr. Mürdter, is working with what are known as organoids: artificial mini-tumors grown, for instance, in a gel extracted from mouse tumors. “Tumor avatars” is Dr. Mürdter’s name for them.
Mini-tumors grow in different colored fluids. Some can even be seen with the naked eye, resembling a tiny, harmless-looking piece of flesh. “These organoids allow us to track how a tumor behaves in a living body to a pretty good degree of accuracy,” says Dr. Mürdter. "For instance, we can check which substances a tumor will respond to, which it builds up resistance against, and which cause it to shrink in the long term."
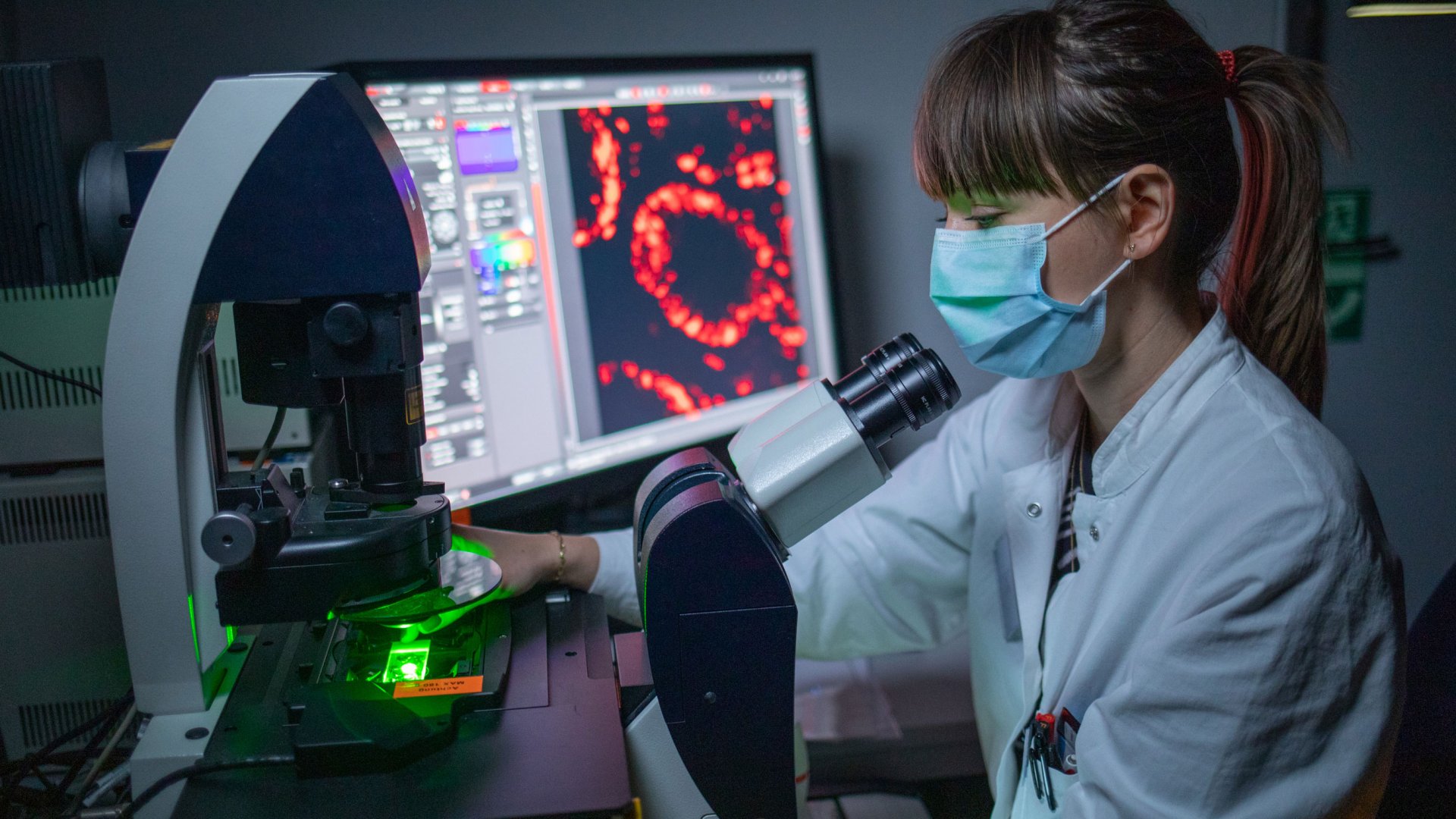
The IKP pools all different kinds of specializations. “These days, we can carry out genetic analysis within half an hour,” explains Dr. Mürdter. With the help of a laser microscope, tumors and organoids can be observed in the nanometer range, while the mass spectrometers down in the lower basement can detect almost any substance in any dilution. All of this comes together in a relatively small space with everything close together. Equally, all employees know and are on familiar terms with one another – they’re all on the same page with one goal in mind.
But there’s another factor behind the fact that translation is practiced so purposefully at the IKP, namely the Institute’s close links to the Robert Bosch Hospital’s Oncology Center. Tumor samples are delivered straight from the operating theater several times a week before being cut into 0.3-millimeter slices and sent for further processing, for example into organoids. As we speak, research is in full swing into breast, intestinal, and ovarian tumors above all.
But the team is also very often busy with lung cancer, whose high number of variants and mutations makes for particularly interesting core oncological research. “It’s a question of give and take between treatment and research,” says Mürdter. “We get the patients’ tumor material, and, in return, we strive to ensure the latest research findings are incorporated back into their treatment as quickly as possible.”
“We saw a tiny chance, and we jumped on it.”
This may well have been how Ms. Sonnleitner’s tumor samples ended up in the IKP’s underground labs. In her words, the fact she’s still here to talk about her illness in person is a miracle: “I didn’t want a prognosis, I asked the doctors not to give me a life expectancy,” she says, “but I didn’t feel I had long left: the pain, the cough, the depression – I just couldn’t take it anymore.”
But after taking this new drug, the inhibitor selpercatinib, she woke up the next morning with a remarkable improvement: “I wouldn’t say I was symptom-free, but I was only in a quarter as much pain as I had been. My husband got a bit of a shock when he walked in and saw me sitting up in bed, not lying down.” The improvements stabilized and even the metastases are receding. “I’m still not well,” says Ms. Sonnleitner, “and I might never win my battle with cancer. But being able to live a relatively pain-free life, most of all without that nagging cough, is the greatest gift of all right now.”
Professor Dr. Kopp, too, is very pleased: “We saw a tiny chance, and we jumped on it. Now we have to see how things play out. Some inhibitors only work in the short term before the tumor develops resistance strategies that we need to counteract. Research into this is currently in full swing,” he adds.
"I have never felt alone with my illness."
Melanie Sonnleitner has complete faith in the team at the Robert Bosch Hospital. “I had a lot of respect for hospitals before I got sick,” she says. Going into hospital literally gave her heart palpitations.
Once she was diagnosed with cancer, it became clear to her that “I only stand a chance if I give everything to the treatment. But the team here makes it easy for me. Not only are they incredibly well-informed, they also welcomed me with open arms. I have never felt alone with my illness.” Perhaps that is exactly what translation is all about: ensuring no one is left alone with their illness, that everything works together with the goal of healing.